Covid-19: Can Melatonin and Vitamin D help?
Right now, there is pretty much one topic: Covid-19. Many hope for a vaccine, but it’s not less important to find a treatment and others way to prevent infection. The internet is full of advise on how to boost the immune system. Some of it is good, some of it is crap, some of it is simply a way for other people to make money. So I got the idea to show people how to boost the immune system with light, darkness and good sleep. It is low cost and has few side effects, but so far, not too many people talk about light as a health factor.
Initially I thought about melatonin, but I also wanted to have a look at the “sun vitamin” D. I had no idea that I would get right into a lively discussion concerning Covid-19. While media mostly talk about Chloroquin and Remdesivir, some researchers have already connected the threads and even done some research that shows how Covid-19 can be helpful with prevention and treatment of Covid-19.
To be absolutely clear: None of these hormones will protect you on its own from Covid-19. They are no miracle cures to become healthy again. But the right use of light, and a sufficient supply of melatonin and vitamin D can help your body to fight SARS-Cov2 and might make a difference in the outcome if you catch Covid-19. They can even improve the chances in severe cases when added to other drugs.
What SARS-Cov2 does in our body

SARS-Cov2 is a coronavirus. Most of them are pretty harmless, but the severe diseases SARS (2003) and MERS (2013) have also been caused by coronaviruses. Fortunately, they have been contained quickly. SARS-Cov2 is especially problematic for elderly people and people with cardio-vascular diseases, pulmonary diseases, a suppressed immune system, obesity, diabetes, cancer, as well as smokers. Men have a higher risk for severe cases than women.
Our knowledge of SARS-Cov2 is constantly increasing and by now we have a much better understanding of the disease. The virus enters our body through the respiratory passages an settles down in the walls of the alveoli in our lungs, where it causes symptoms similar to pneumonia. This causes fluid to leak into the alveoli, oxygen can’t enter the blood anymore and the patient needs ventilation. It then moves into the blood vessels, where it triggers inflammation. It also causes blood clots which block the vessel and prevent oxygen transport[1], while bigger clots can cause lung failure, heart attacks or strokes.
In many patients, Covid-19 causes a cytokine storm. Cytokines are a group of substances including interleukines and interferones which are released by macrophages, cells of the inate immune system. They trigger inflammation and fever to support the immune system. The release of too many cytokines can cause a cytokine storm with uncontrolled inflammation. Fluid leaks into the lungs and blocks oxygen exchange with the blood. The result can be acute respiratory deficiency syndrome (ARDS) and finally death.
Covid-19 is a disease with many faces and many mysteries for physicians. Scientists unrevell these mysteries bit by bit on their search for a treatment. In addition to several synthetical drugs, two hormones might be of use: melatonin and vitamin D. Let’s have a look what they do and how they might help with SARS-Cov2.
Melatonin, the hormone of darkness

When the sun has set, our brain starts to produce the hormone melatonin. Almost all physiological processes in our body follow a day-night-rhythm which is controlled through melatonin. Blue-rich light from the sun or from LED-displays in computers, smartphones, tablets, or eReaders blocks its production.
Melatonin brings our body into a state of rest and regeneration. It is therefore often called the “sleep hormone”. There is no restful sleep without it. Our immune system doesn’t work well without sufficient sleep. If you regulary sleep less than six hours per night, you have an increased risk for obesity and high blood pressure – both risk factors in Covid-19 – and your immune response is significantly reduced.
Melatonin itself is also an important part of the immune system. Russell Reiter, who has been studying melatonin since the seventies, thinks that there are several options to use melatonin against Covid-19 [2]. And he is not the only one.

Melatonin is an active component of the inate immune system. Long before antibodies are produces, viruses and bacteria are attacked and destroyed by macrophages. Melatonin is one of the substances that activates the macrophages. It is also involved in the release of cytokines, which trigger inflammation. In mild cases of Covid-19, this defense seems to be enough to stop SARS-Cov2. Melatonin is also anti-inflammatory: After enough cytokines are present, melatonin will stop the release, thus reducing the risk of a life-threatening cytokine-storm [3]. Melatonin application has been shown to redcue the cytokine-levels [4] in patients with diabetes, multiple sclerosis and acute inflammation.
If the inate immune system is not successful, the adaptive immune system kicks in – again with the help of melatonin. Cells that have been infected with a virus present virus-proteins, so called antigens, on their surface. These antigenes are used by lymphozytes to produce anti-bodies. Lympozytes can also destroy the infected cells.

Naturally, the virus will try to trick the lymphocytes, and indeed there is some evidence that Lymphozyten are blocked by SARS-Cov2 [5]. In an Australian case study [6], a patient recovered after the amount of lymphocytes had increased. Melatonin is a vital component in the production and differentiation of lymphocytes. Without low amounts of melatonin, no sufficient amount of lymphocytes can be produced.
Another problem of SARS-Cov2 is that the virus impairs the regulation of the blood pressure. It has been shown in animal experiments that melatonin relaxes the blood vessels and reduces blood pressure [7].
A general problem in viral infections is the production of free radicals, highly active molecules that destroy cells. In Covid-19, they are the cause of massive damage in lung tissue and blood vessels. Melatonin is a first-class antioxidant [8], which binds about ten-times as many free radicals than vitamin C or E. It is also active in the brain, different to vitamins which can’t cross the blood-brain-barrier. Therefore, a good portion of melatonin is more useful than oranges or goji-berries – and considerably cheaper.

A high amount of free oxygen radicals are produced due to artificial ventilation, when the patient breaths in high oxygen concentrations. This causes scar tissues in the lung and thus pulmonary fibrosis, a common after-effect even in mild cases of Covid-19. In 2005, a study on newly born babies showed that melatonin reduces the inflammation and damage cause by free radicals [9]. It is also known how melatonin is protecting lung tissue [10].
There might be another reason to treat patients in intensive care with melatonin. The pain and fear are immense. This stress increases the risk to die and leaves psychological scars. In a study from 2015, melatonin reduced the amount of sedatives needed for the patients [11]. In another study, sleep improved [12], a great relieve and help for someone, who fights for ones life.

Melatonin on its own will not heal Covid-19, but it can support other drugs. Based on several studies, Alex Shneider [8] is convinced that melatonin could increase the effect of Remdesivir, Ribavarin, Chloroquin/Hydroxychloroquin and Methylprednisolon and reduce their side-effects. For this reason he asks for clinical trials, especially since melatonin has two advantages: It is a cheap drug and, more important, the only side-effects in a short-term treatment, even with high doses, are tiredness and lack of concentration.
Melatonin is obviously a multifunctional part of our defence against SARS-Cov2. But do we actually have enough of it in our bodies? Probably not, although actual studies of melatonin levels haven’t been done yet. Melatonin is only produced in darkness, but we spend our evenings with artificial light, gaze into blue-rich LED-displays until late at night, and even our bedrooms are brighter than they should be. Additionally, we don’t get enough sunlight during the day, though this is needed to produce serotonin as source of melatonin. Serotonin, the “happiness hormone” itself would be great right now, because it brightens our mood, calms fear, and reduces aggressions. Instead, we spent most of our days indoors.
Especially elderly people have a lack of melatonin. There is a natural reason for this, because our body produces the highest amount of melatonin when we are children. The older we get, the less melatonin we produce, no matter how much sunlight and darkness we get. This is one of the reasons why elderly people suffer from sleep problems so often. It is even worse for people living in nursing homes or staying in hospitals. The rooms are gloomy during the day, and at night, the dim light from the corridors keeps away the healthy darkness. This fits into the pattern of Covid-19, which is especially dangerous for elderly people. It is also interesting that the risk factors for Covid-19 – cardiac problems, respiratory diseases, diabetes and immune deficits – are all related to a lack of melatonin. Simply a coincidence?
Vitamin D, the hormone of the sun
Sun light is not only needed for the production of serotonin, but also for vitamin D. Most people connect vitamin D with strong bones, but it is also a vital part of our immune system and – especially important for Covid-19 – in the regulation of our blood pressure. So it’s no surprise that in the last weeks a lively discussion about the vitamin D and Covid-19 is going on between scientists and doctors. There are even some promising studies out yet.
It has been known for a while that there is a connection between vitamin D and respiratory infections. A meta-study [13] by Martineau et al., published in Lancet, looked at 25 studies with more than 11.000 participants. Taking vitamin D supplements on a regular basis or having a sufficient vitamin-D-status due to sun exposure reduced the risk for respiratory infections.

However, far too many people do not have enough vitamin D. We don’t spent enough time in the sun and if we do, we protect ourselves from UV-B, since it is the cause of sunburn. To get enough UV-B for vitamin D production, we need to be in the sun around noon – the very time we are told not to go out to prevent sunburn.
While many health organisations define 20 ng/ml as sufficient vitamin D level, evidence is mounting that 30 ng/ml would be a better value. In several European countries, average vitamin-D-levels are below these recommendation. It is more common in elderly people, and elderly men are even more affected, because elderly women often take vitamin-D-supplements to prevent osteoporosis. Let’s remember: elderly people and especially men are more at risk to die from Covid-19.
There is also a seasonal variation in vitamin-D-levels. In winter, not very surprising, vitaim-D- levels are lower, for once because the sun is lower in the sky and less UV-B passes through the atmosphere, but also because of the cold. We are not as keen to spent much time outdoors and if we do, we wear lots of clothes. Bare skin in winter? Brrrrr…….
Three british scientist[14] compared the number of European people who died from Covid-19 in March with the average vitamin-D-level of their country. This, as they say themselves, rather crude study indeed found a significant correlation. The highest death rate was found in Italy and Spain, countries with considerably lack of vitamin-D. This might be surprising at first, since these countries have lots of sun, but people there actually avoid being in the sun because it is too strong. Low death rates were found in Denmark, Norway, and Finland, countries in which people eat lots of fat and vitamin-D-rich food and regularly take vitamin-D-supplements.
The idea that lack of vitamin-D might be an essential factor for the severeness of Covid-19 has also been voiced by researcher Murat Kara and colleagues [15] from Turkey and an US-American team around William Grant [16]. Their idea is supported by a retrospective study from Switzerland [17]: people tested positive for SARS-Cov2 had significantly lower vitamin-D- levels than those tested negative. The authors think that Vitamin D might lower the infection risk.

There are also two pre-prints of studies published at SSRN showing a correlation between the actual vitamin-D-status of a patient and the severness of the disease. An Indonesisan study [18] found a 10-times higher risk to die in patients with vitamin-D-deficit, while a Philippinian study [19] on 212 patient found that those with vitamin-D-levels of 30 ng/ml or higher had a 20-times higher chance to be a mild case.
Even IUC patients could profit from vitamin D. In an US-american study [20] on 31 ventilated patients, vitamin D significantly reduced the time they spent in the hospital.
Similar to melatonin, there are several functions of vitamin D that explain these positive outcomes. It is involved in the activation of macrophages and regulation of cytokin-release. It is therefore an important part of the immune system and can reduce the risk of a cytokin-storm.
But there is another promising aspect of vitamin D in relation to Covid-19: the ACE2-receptor, which is the entry-point for SARS-Cov2. The ACE2-receptor is responsible for relaxing and widening the blood vessels and lowering the blood pressure, especially at the heart. It is also anti-inflammatory and protects the lung. For these reasons, blocking the ACE2-receptors increases the risk of heart attacks, strokes, and acute lung failure, the most common causes of death in Covid-19 patients. By the way, ACE2 also was the entry-point for SARS-Cov1, the virus that caused SARS. It was shown back then that the lungs of mice with a high amount of ACE2-receptors were less damaged by SARS [21].
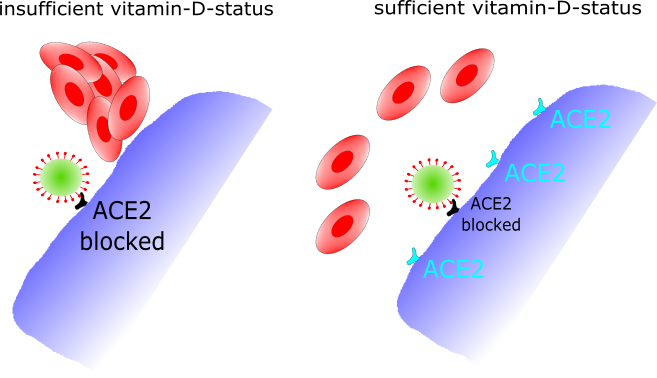
Vitamin D has been shown to increase the number of ACE2-receptors [22] and thus keeping up their function in blood pressure regulation. Additionally, the ACE2-receptor is part of the production of antioxidants, so a high number of ACE2-receptors is a better protection against free radicals.
The number of ACE2-receptors is lower in men and elderly people. ACE2 is also involved in cardiovascular and pulymonary diseases, diabetes, and obesity, so once again there is a link to Covid-19 risk groups. An elevanted blood pressure is also an increased risk for the lungs. These are many good arguments for sufficient vitamin-D-levels, and there is need for clinical studies on the use in severe cases of Covid-19. Especially since there are two very strong arguments for vitamin D: it is cheap and side-effects only occur with high doses.
So what can you do yourself?
I have summarised many arguments to use melatonin and vitamin D in a clinical situation. None of these two substances offers an absolute protection, but both can help to fight SARS-Cov2. So for everyone of us it is a good idea to work on good amounts of both hormones right now.
Rose Anne Kenny [23], health expert at University Dublin, Irland, sums up the situation for vitamin D in these words: “The circumstantial evidence is very strong […] we don’t have randomised controlled trial evidence, but how long do you want to wait in the context of such a crisis? We know vitamin D is important for musculoskeletal function, so people should be taking it anyway.”
Adrian Martineau [23], author of the Lancet-study that found a positive effect of vitamin D as protection against respiratory infections [13], recommends the use of vitamin D, even if it is only one of many factors influencing the outsome of Covid-19 in a patient.
But what can we do ourselves – especially since I have promised you solution without extra costs? Vitamin D is a fat-soluble substance and found in fatty fish like herring or salmon, also, though in lesser amounts, in liver and egg yolk. It is not possible to get enough vitanim D through food. We need to get it from the sun!

In Central Europe, sunlight between March and October contains enough UV-B to produce vitamin D, but only around noon. Shade, clouds, and sun screen reduce the amount of UV-B. There are different recommendations about the length of sun bathing you need to produce enough vitamin D, ranging from 5 to 25 minutes daily, to 30 minutes twice a week with bare face, hands, arms, and legs. In any case, it should be shorter than 30 minutes to prevent sunburn and you should consider your personal skin sensitivity.
If you got enough vitamin D during summer, it can get you through winter, if not you can ask you doctor or pharmacist about supplements. Be careful here, because there is no legal maximal dose. If you take more than 4,000 I.E., especially for a longer time, this can interrupt your calcium-balance and cause vomitting, diarrhea, head ache, pain in your joints, kidney stones and in severe cases even heart problems. Freely available products have repeatedly causes intoxications due to higher vitamin-D-contact than stated on the label [24]. The correct dose has been a matter of discussion for quite some time, so please talk to your doctor or pharmacist. You can even check your vitamin-D-status to be on the safe side.
Melatonin is only produced during dark nights, though brights days are important too. To get a healthy amount of melatonin and day-night-rhythm, spend at least part of your days in bright areas, even if you are indoors. On sunny days, the light in shady areas is still enough. In a time of dim days you can use a daylight lamp, but only in the morning. Ideally, you are still in bed at sunrise.
At night you should keep light low, and stay away from blue-rich light from LEDs and CFLs, because they supress melatonin production. Use light sources with less than 2700 Kelvin (warm-white, better amber, or vintage). If you use a computer, tablet, smartphone or eReader, switch on the night mode and reduce the brightness. Switch off electronical devices one or two hours before bedtime.
Try to keep your bedroom as dark as possible without feeling uncomfortable. The darker the room, the more melatonin will be produced. Some people are so distracted by light that they can’t fall asleep if there is a small dot on the wall. If possible, follow your individual sleep-wake-cycle instead of using an alarm-clock and sleep as much as you need to feel awake in the morning. Six hours each night is the absolute minimum, seven to eight are advisable. There are individual variations in the best time for sleep, depending if you a an early or late person. If you want to know more about sleep and light, check out my blog post Light and sleep – or why we (usually) sleep at night.
Many biologists and doctors are cautious about melatonin supplements. Do not take them without consulting your doctor. If you buy supplements, your body might not be able to absorb the amount of melatonin promised to you, because many supplements have a low bioavailabilty. If you take Melatonin during the day, it can interfer with your natural day-night-rhythm, which can actually interfere with your health in many ways. Possible side-effects are fatigue and lack of concentration, artificial melatonin can also reduce your natural melatonin production. Try to produce your own melatonin with a smart light regime first before you consider artificial supplements.
Conclusion

Our body has evolved in a constant rhythm of day and night, light and darkness. The sun hormone vitamin D and the darkness hormone melatonin are vital tools to protect our body against diseases. We are now at the beginning of summer, and though we will have to deal with many restrictions to protect us from SARS-Cov2, we should use every opportunity to charge up on sun light. At night, darkness can provide rest and recreative sleep. If we follow the rhythm of life and allow our hormones to do their work, if we even manage to build up a storage for winter, we will have a better defence against SARS-Cov2. And the best thing about it: sun and darkness don’t cost any money and are good for us in many ways!
References
- Ackermann et al. 2020. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. New England Journal of Medicine
- Anderson & Reiter. 2020. Melatonin: Roles in influenza, Covid-19, and other viral infections. Reviews in Medical Virology 30: e2109.
- Reiter et al. 2020. Melatonin Inhibits COVID-19-induced Cytokine Storm by Reversing Aerobic Glycolysis in Immune Cells: A Mechanistic Analysis. Medicine in Drug Discovery 6: 100044.
- Zhang et al. 2020. COVID-19: Melatonin as a potential adjuvant treatment. Life Science 250: 117583.
- Wang et al. 2020. SARS-CoV-2 infects T lymphocytes through its spikeprotein-mediated membrane fusion. Cellular & Molecular Immunology. doi.org/10.1038/s41423-020-0424-9.
- Thevarajan et al. 2020. Breadth of concomitant immune responses prior to patient recovery: a case report of non-severe COVID-19. Nature Medicine 26: 453-455.
- Herrera & Gonzalez-Candia. 2020. Comment on Melatonin as a potential adjuvant treatment for COVID-19. Life Sciences.
- Shneider et al. 2020. Can melatonin reduce the severity of COVID-19 pandemic? International Reviews of Immunology:1-10.
- Gitto et al. 2005. Correlation among cytokines, bronchopulmonary dysplasia and modality of ventilation in preterm newborns: Improvement with melatonin treatment. Journal of Pineal Research 39(3):287-293.
- Zhao et al. 2020. Melatonin protects against lung fibrosis by regulating the hippo/YAP pathway. International Journal of Molecular Sciences 19(4).
- Mistraletti et al. 2015. Melatonin reduces the need for sedation in ICU patients: A randomized controlled trial. Minerva Anestesiologica 81(12): 1298-1310.
- Lewis et al. 2018. Melatonin for the promotion of sleep in adults in the intensive care unit (Review). Cochrane Database of Systematic Reviews 2018(5): CD012455.
- Martineau et al. 2017. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ 356: i6583.
- Ilie eta l. 2020. The role of Vitamin D in the prevention of Coronavirus Disease 2019 infection and mortality. Aging Clinical and Experimental Research: 0123456789.
- Kara et al. 2020. ‚Scientific Strabismus‘ or Two Related Pandemics: COVID-19 & Vitamin D Deficiency. British Journal of Nutrition 12: 1-20.
- Grant et al. 2020. Evidence that vitamin d supplementation could reduce risk of influenza and covid-19 infections and deaths. Nutrients 12(4): 1-19.
- D’Avolio et al. 2020. 25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2. Nutrients 12(5): 1-7.
- Raharusun et al. 2020. Patterns of COVID-19 Mortality and Vitamin D: An Indonesian Study. SSRN.
- Alipio. 2020. Vitamin D Supplementation Could Possibly Improve Clinical Outcomes of Patients Infected with Coronavirus-2019 (COVID-19). SSRN.
- Han et al. 2016. High dose Vitamin D administration in ventilated intensive care unit patients: A pilot double blind randomized controlled trial. Journal of Clinical and Translational Endocrinology 4: 59-65.
- Kuba et al. 2006. Angiotensin-converting enzyme 2 in lung diseases. Current Opinion in Pharmacology 6(3): 271-276.
- Cui et al. 2019. Vitamin D receptor activation regulates microglia polarization and oxidative stress in spontaneously hypertensive rats and angiotensin II-exposed microglial cells: Role of renin-angiotensin system. Redox Biology 26: 101295.
- Mitchell. 2020. In Focus Vitamin-D and COVID-19: do deficient risk a poorer outcome? Lancet 8587(20):30183.
- Taylor & Davies. 2018. A review of the growing risk of vitamin D toxicity from inappropriate practice. British Journal of Clinical Pharmacology 84: 1121-1127.


